Comorbidity And Its Impact On Patients With COVID-19
By Uduak Effiong
Coronavirus disease (COVID-19) is a global pandemic caused by severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2). This pandemic started in Wuhan, a major city in China, and has spread to more than 180 countries. Coronavirus is affecting people of all ages, but older patients are at more risk of developing a severe type of COVID- 19 illness due to their associated comorbidities (conditions like diabetes).
According to a study conducted in China showed 133 people out of 344 patients died on the 28th day and 141 patients suffered from comorbidities associated with Covid-19 including hypertension.
Similarly, another study demonstrated that out of 633 Covid -19 patients 247 patients developed at least one comorbidity. This study also indicated that, 60 years old people were particularly expected to develop the more serious form of COVID-19 disease.
Comorbidities Impact On Covid-19 Patients
Coronavirus is a relatively novel and understudied illness, the available evidence about Coronavirus is also limited. However, based on some case reports, it is safe to assume that comorbidities such as kidney problems, blood pressure, diabetes, liver disease, lung disease, cancer can increase the risk of Covid-19 infection in patients.
Similarly, in the elderly population, cardiovascular disease, diabetes, or lung disease are common which places them at higher risk of acquiring more severe sickness, and an increased risk of dying if they catch an infection like COVID-194.
It is also important to mention here, that patients with respiratory illnesses like asthma are at a disadvantage because coronavirus severely affects respiratory tracts, which leads to an increase in asthma attacks, acute respiratory distress, and pneumonia.
According to the CDC’s weekly report on morbidity and mortality, 34.6 percent of patients ages of 18 to 49 years had chronic lung illness, like asthma5. Additionally, HIV-positive patients with lower CD4 count and people not receiving anti-retroviral treatment are at more risk of developing additional medical problems, including COVID-19.
Similarly, according to the “International Aids Society”, HIV-positive people, individuals on antiretroviral therapy, and patients with higher CD4 count are at higher risk of contracting COVID-19 infection as those who are HIV negative
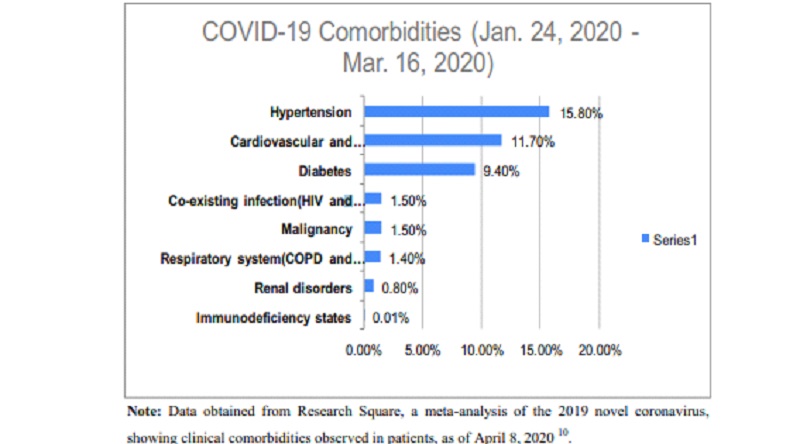
Furthermore, data from the research shows that 15.8% covid-19 patients had hypertension, 9.40% of patients had diabetes, 1.40% of individuals had COPD.
Commodities reported in Covid-19 patients and death percentage
Comorbidities Death percentage
Hypertension 55.4%
Hyperlipidemia 18.5%
Diabetes 37.3%
Renal disease 11.0%
COPD 8.3%
Coronary artery disease 12.4%
Cancer 8.1%
Dementia 9.1%
Atrial Fibrillation 7.1%
This data is taken from hospitals and nursing facilities from New York, as of April 6, 2020. This data shows that 55.4% of patients with hypertension died due to COVID-19 Infection. Moreover, 8.3 individuals suffering from COPD died because of COVID-198. Therefore, it can be concluded that patients with comorbidities can acquire more severe form Covid-19 infection which leads to their death.
References
⦁ Wang Y, Lu X, Chen H, Chen T, Su N, et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. AJRCCM. 2020; 201:1430–1434.
⦁ Zhang J, Wang X, Jia X, Li J, Hu K, et al. Risk factors for disease severity, unimprovement, and mortality of COVID-19 patients in Wuhan, China. Clin Microbiol Infect. 2020;26:767–772. DOI: 10.1016/j.cmi.2020.04.012.
⦁ CDC. Coronavirus (COVID-19): symptoms of coronavirus. Centers for Disease Control and Prevention. 2020. [Accessed April 18, 2020, https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html].
⦁ BCCDC. COVID-19 vulnerable populations. British Columbia Centre for Disease Control. 2020. [Accessed April 18, 2020, http://www.bccdc.ca/health-info/diseases-conditions/covid-19/vulnerable-populations].
⦁ Garg S, Kim L, Whitaker M, O’Halloran A, Cummings C, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 states, March 1–30, 2020. Centers for Disease Control and Prevention: MMWR. 2020;69(15):458–464.
⦁ IAS. COVID-19 and HIV: what you need to know. The International AIDS Society. 2020. [Accessed April 20, 2020, https://www.iasociety.org/covid-19-hiv].
⦁ 20. WHO. Q&A on COVID-19, HIV, and antiretrovirals. World Health Organization. 2020. [Accessed April 20, 2020, https://www.who.int/news-room/q-a-detail/q-a-on-covid-19-hiv-and-antiretrovirals].
⦁ Sanyaolu, A., Okorie, C., Marinkovic, A., Patidar, R., Younis, K., Desai, P., Hosein, Z., Padda, I., Mangat, J., & Altaf, M. (2020). Comorbidity and its Impact on Patients with COVID-19. SN comprehensive clinical medicine, 1–8. Advance online publication. https://doi.org/10.1007/s42399-020-00363-4.
